The Food and Drug Administration on Wednesday approved the sale of an antibiotic to treat urinary tract infections in women, giving U.S. health care providers a powerful new tool to fight a common infection that is increasingly resistant to the existing suite of antimicrobial drugs .
The drug, pivmecillinam, has been used in Europe for more than 40 years, where it is often first-line therapy for women with uncomplicated urinary tract infections, meaning the infection is confined to the bladder and has not reached the kidneys. The drug will be marketed in the United States as Pivya and will be made available by prescription to women aged 18 and older.
It's the first time in two decades that the FDA has approved a new antibiotic for urinary tract infections, which affect 30 million Americans each year. Urinary tract infections are responsible for the greatest use of antibiotics outside of the hospital environment.
“Uncomplicated urinary tract infections are a very common condition affecting women and one of the most frequent reasons for antibiotic use,” Dr. Peter Kim, director of the anti-infectives division at the Center, said in a statement for FDA drug evaluation and research. “The FDA is committed to promoting the availability of new antibiotics when they are proven safe and effective.”
Utility Therapeutics, the US company that acquired the rights to pivmecillinam, said it will be available in 2025. The company is also seeking FDA approval for an intravenous version of the drug that is used for more serious infections and is usually administered in a hospital environment. .
Health workers said they are excited to have another tool in their arsenal given the growing challenge of antimicrobial resistance, which makes existing drugs less effective as pathogens mutate in ways that allow them to survive a course of antibiotics.
According to the World Health Organization, the problem, largely due to the overuse of antibiotics worldwide, is associated with five million deaths.
“This is an exciting new possibility for the treatment of lower urinary tract infections,” said Dr. Shruti Gohil, professor of infectious diseases at the University of California, Irvine School of Medicine, and author of a recent study in JAMA focused on ways to reduce the excessive use of antibiotics in hospitals. “But I would also say that it will be important to use the drug responsibly in this country so that we don't generate resistance against it.”
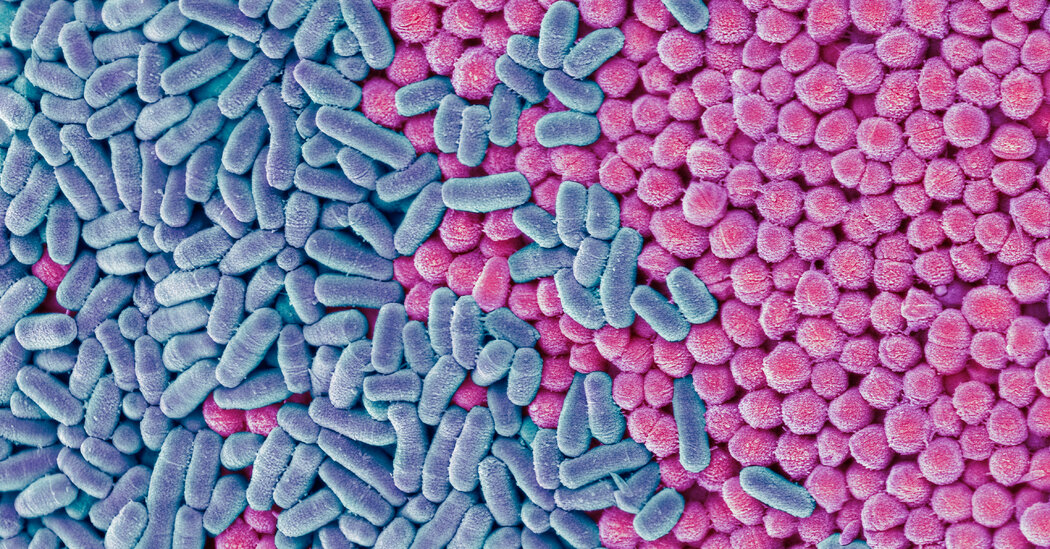
Most urinary tract infections occur when bacteria such as E. coli travel from the rectum, genital area, or vagina into the urethra and enter the bladder. As they multiply, the pathogens can cause abdominal cramps, burning, and bloody urination.
More than half of women in the United States will get a UTI in their lifetime, compared to 14 percent of men. This is largely due to the different architecture of the urinary tract in the sexes: women have a shorter urethra than men, which makes it easier for bacteria to reach the urinary tract.
Most urinary tract infections are now resistant to one or more antibiotics; Ampicillin, once a common treatment, has been largely abandoned. Infections that reach the kidneys or enter the bloodstream are harder to treat and more dangerous.
People with weakened immune systems or chronic medical conditions are usually most vulnerable to drug-resistant infections. But urinary tract infections have a dubious distinction: They pose the greatest risk to healthy people due to drug-resistant germs.
In the four decades since it was first approved for use in Europe, Pivmecillinam has been prescribed more than 30 million times, mostly in Nordic countries, with few reported complications.
The FDA said nausea and diarrhea were the most common side effects in the clinical trials that paved the way for pivmecillinam's approval in the United States.
Tom Hadley, president and chief operating officer of Utility Therapeutics, said his company moved to acquire U.S. rights to pivmecillinam after Congress in 2012 granted five more years of exclusivity to makers of new antimicrobial drugs.
Henry Skinner, managing director of the AMR Action Fund, a venture capital fund that invested in Utility Therapeutics' attempt to bring pivmecillinam to the United States, said he was gratified by the FDA approval but said the long-term prognosis deadline for new antimicrobial drugs remains unchanged. gloomy. The $1 billion fund, funded by the pharmaceutical industry, invests in biotech start-ups working on promising antimicrobials.
Most of the nation's largest drugmakers, unable to profit from antibiotics, have long since abandoned the field, he said, and a paucity of investment has prompted an exodus of talented researchers.
A federal initiative that would create a subscription-based model for antibiotic development languishes in Congress. The $6 billion measure, the Pasteur Act, would provide drug companies with an upfront payment in exchange for unlimited access to a drug once approved by the FDA
Mr Skinner said he was haunted by a recent estimate that drug-resistant infections could claim 10 million lives by 2050.
“There are definitely bright spots,” he said. “But today more people are dying than they should because we are going backwards and not providing the doctors, drugs and diagnostics needed to address the antimicrobial resistance crisis.”